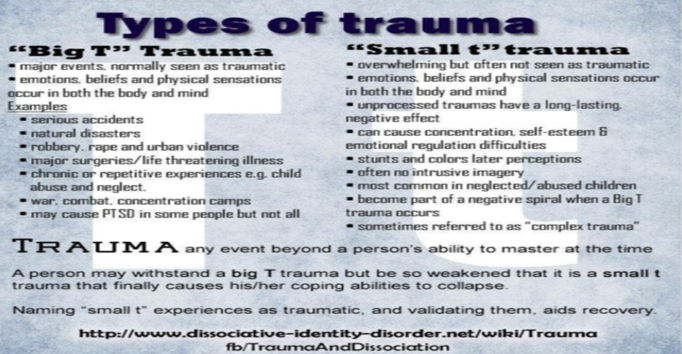
On 27th June each year, the UK raises awareness of post traumatic stress disorder (“PTSD”) – let’s just call it trauma. Many clients we see come with symptoms of chronic ill health, anxiety, low mood/depression, OCD, eating disorders, intrusive thoughts, feeling disconnected from others, struggling to concentrate and remember things, addictions to food, alcohol, prescription and non-prescription drugs, gambling, emotional control difficulties eg anger, irritability. It’s often a surprise when we mention the phrase ‘trauma response’ to sum up their symptoms as many assume that trauma only comes from working in jobs such as the emergency services or military; or it only happens if we have been involved in a catastrophic event eg a bombing or serious accident where someone dies. When we start talking to clients about their life experiences in terms of small ‘t’ and big ‘T’ traumas – ranging from witnessing a loved one being seriously ill or dying, living with bullying, learning that your lifelong partner has had an affair, losing their career, they begin to understand how their survival response to life events impacts on them now.
What are common trauma symptoms?
In children, we can witness a regression into an earlier stage of childhood physically such as bed-wetting, sleep problems, changes in appetite, tantrums, forms of self-harm. In adults, we can respond in similar ways by withdrawal, being sluggish and demotivated or overactivity such as over-working, feeling agitated/angry and being unable to slow down. This can lead to ways of coping that help with numbing feelings such as addictions and dissociation. The body can go into hypoactivity or hyperactivity and this is where we see a cross-over into ADHD (“Attention Deficit Hyperactivity Disorder”) https://psychcentral.com/adhd/adhd-and-trauma. Physical health problems range from general problems in the gut, muscular pain, headaches to more serious chronic health problems such as auto-immune disorders, heart disease and cancer.
Trauma is not what happens to a person, but what happens within them. It’s also what didn’t happen to them which should have happened often where essential human needs are not met. This can be psychological/emotional neglect or physical needs such as food, warmth, and a safe home. Gabor Mate explains this simply. https://www.youtube.com/watch?v=nmJOuTAk09g
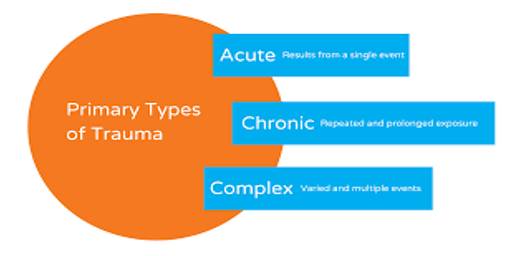
There are 3 types of trauma – acute (single event), chronic (repeat of similar events) and complex (multiple events and types). Often small ‘t’ traumas that are repeated over a period of time are not seen as significant by clients.
When something negative happens, we can respond to this in a variety of ways – some of which are unhelpful such as self-blaming, feeling guilt, shame, avoiding and retreating from life. Many clients with traumatic experiences talk about having low self-esteem which comes from feeling as if they were in some way at fault or to blame for what happened. We often develop very generalised negative thoughts about ourselves and the world and our thinking becomes less flexible and rigid. This then leads to a negative spiral as we go into current situations with a tainted perception rather than a neutral or positive view of what may happen. There is often an unseen link between childhood trauma and later mental health problems that is called latent vulnerability. This is where the cumulative impact of negative life events can remain hidden and build up over time.
In line with its Greek origins the word trauma means a wound – an unhealed one. Typically, at the time of the wounding we didn’t have the right resources so the person is compelled to defend themselves by denying feeling. Often others around us also denied or tried to minimise our right to feel. Whilst we can’t change what happened to us in the past, we can validate, acknowledge with compassion and now provide ourselves with the resources that we need to process that past event in a healthy way (rather than continuing to disconnect from it). This can be done in talking therapy and other forms of creative expression such as creative writing/art/music, pilates/yoga/dance, meditation/mindfulness practice to name a few.
How can talking therapy help?
EMDR (“Eye Movement Desensitisation Reprocessing”) therapy is a NICE (“National Institute for Health and Care Excellence”) guideline approved treatment for trauma alongside CBT (“Cognitive Behavioural Therapy”). I have incorporated EMDR into her clinical practice for 7 years and clients with a variety of traumatic experiences from one-off incidents such as life-threatening health situations/car accidents to childhood abuse experiences report significant benefits. It offers a way of processing traumatic experiences which are often stuck in the mind-body and reduces symptoms of trauma by changing how memories are stored in your brain.
Dissociation and feeling disconnected from ourselves/others/our environment are one way that the brain helps us cope with traumatic experiences as they have happening to us. By the brain shutting off this is one way that we survive chronic stress. We don’t have a choice about this as it is an automatic survival response and many clients talk about having periods in their life when they don’t remember significant events. Whilst this is positive at the time, dissociation as a coping mechanism can cause us difficulties long term and make us feel disconnected from others and our lives in the present day. We lose out on feeling deeply connected to our significant others and enjoyment in life causing depression and relationship difficulties. Relationship crisis is a reason that many people come into therapy often a long time after trauma has been experienced.
One of my past clients, Scott, has kindly agreed to share his experience of EMDR treatment.
Scott says “I was off work suffering from anxiety and some form of depression. I had low self-esteem and had been having intrusive thoughts. Therapy identified PTSD from traumatic childhood and events linked to work. At the time I was a serving police officer. Rachel suggested EMDR treatment, which I gladly accepted. EMDR treatment doesn’t require any equipment so can be done wherever you are comfortable – online or in person at a clinic and I had both. I went through an EMDR session for each identified traumatic episode. I can honestly say that the treatment worked wonders for me. I was able to get back to work after a long period of sickness. I got my life back.”
Two recent documentaries are available about how EMDR works – one featured Prince Harry having an EMDR session https://www.youtube.com/watch?v=jgWvd67VKaY and BBC journalist, Fergal Keane’s Living with PTSD https://www.bbc.co.uk/programmes/m0017795
There is a wide variety of self-help resources out there such as PTSD UK’s blog https://www.ptsduk.org/, for young people https://www.youngminds.org.uk/young-person/mental-health-conditions/ptsd/
Further information:
https://emdrassociation.org.uk/
Recommended books:
The Body Keeps the Score, Bessel A van der Kolk
The Body Remembers, Babette Rothschild
Waking the Tiger: Healing Trauma, Peter Levine
Getting Past Your Past, Francine de Shapiro
Take a look on our website https://thewellnessconsultancy.org for helpful guidance or contact us for support and advice – email: wellness-consultancy@outlook.com.
Rachel Wesley
Trauma Psychotherapist/EMDR Practitioner

